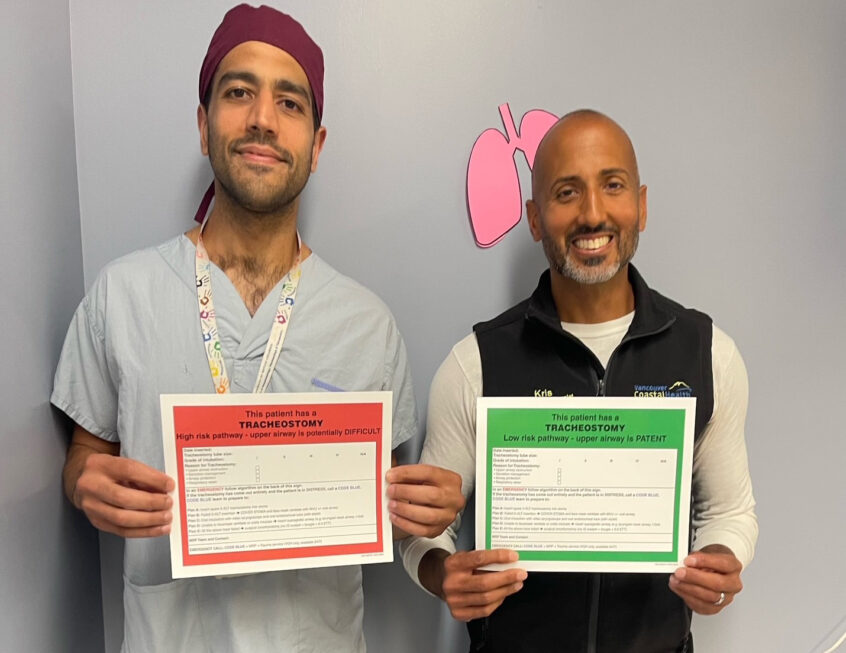
Before joining the Anesthesiology Department at VGH, Dr. Shamir Karmali worked in the UK as a critical physician and anesthesiologist. It was standard practice there for visual cognitive aids to accompany the emergency tracheostomy pack of all patients who had a tracheostomy or laryngectomy. Dr. Karmali believed adopting such a practice here would enhance patient safety. To achieve this goal, he applied for and received funding from VPSA’s Small Steps, Big Idea initiative.
“VGH looks after many patients who need a tracheostomy as part of their care,” said Dr. Karmali. “Multiple surgical services provide this care, with patients going to different areas of the hospital where there is varying expertise in managing tracheostomies. Tracheostomy emergencies on the ward are common and using cognitive aids in emergency management has been shown to improve patient outcomes.”
To achieve his “big idea,” Dr. Karmali had to get buy in from multiple specialist clinical services: anesthesiology, surgery, respirology, nursing, respiratory therapy and the Medical Device Reprocessing Department. He used VPSA’s funding to compensate team members attending project meetings and creating interactive learning materials.
“This is predominantly an educational initiative that will require staff to be trained on the use of the cognitive aids,” said Dr. Karmali. “It was challenging as it involved instituting a change outside of my own usual working environment and sphere of influence. I’m particularly grateful to respiratory therapist Kris Gill and nurse educator Thalia Martens. I relied heavily on them to act as leaders in their own fields and to guide me in what will work or not, and how best to proceed.”
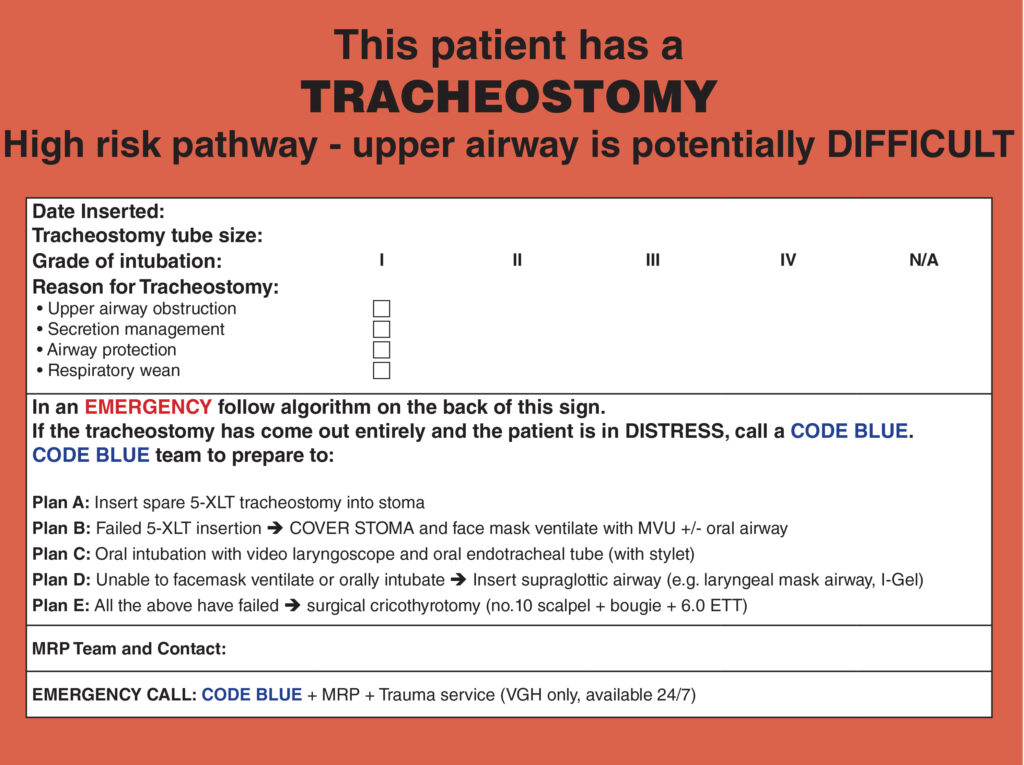 Thanks to this project, every patient having a tracheostomy or laryngectomy performed at VGH now has a visual cognitive aid accompanying their emergency tracheostomy pack. Further, these orders are embedded in CST Cerner so are part of routine workflow.
Thanks to this project, every patient having a tracheostomy or laryngectomy performed at VGH now has a visual cognitive aid accompanying their emergency tracheostomy pack. Further, these orders are embedded in CST Cerner so are part of routine workflow.
The project also had several intangible benefits.
“I’ve developed strong relationships developed with Respiratory Therapy Department at VGH as well as at Lions Gate and Richmond hospitals,” said Dr. Karmali. “This has led to discussion about more collaborative projects to improve patient safety including the potential of introducing qualitative capnography to the wards. I’ve had anecdotal reports the aids have changed or improved timeliness of patient management during emergencies, although this is difficult to study due to the low event rate and need for a provider to take the initiative to provide this feedback. I have received positive feedback from the multidisciplinary team for this intervention, in particular nursing staff.”
Thanks to team members from other disciplines, Dr. Karmali reports that the project has been picked up by other sites within VCH that are keen to roll it out. After this happens, he hopes to collect feedback to assess the confidence of primary responders in managing tracheostomy emergencies on the wards. He anticipates that a continuous cycles of feedback and revisions are likely to be necessary to the visual aids or the workflow.
Do you have an idea that would benefit from project funding? Check out VPSA’s project application process, which begins with a letter of intent from VPSA physician members. Visit this link for more information.
Photo: Anesthesiologist Dr. Shamir Karmali and respiratory therapist Kris Gill holding the visual aids.