Members gathered in person and online September 29 for VMDAS’s most recent quarterly meeting. VMAC Chair Dr. Jennifer Wilson provided an overview of the work of the Vancouver Medical Advisory Committee, after which HAMAC Chair Dr. Jennifer Beaveridge talked about the role of the Heath Authority Medical Advisory Committee. VCH and PHC Chief Medical Information Officer Dr. Eric Grafstein was the final guest speaker at the meeting; he shared updates on the Cerner Patient Portal and AI Scribes.
VMDAS President Dr. Ka Wai Cheung emphasized throughout the meeting the desire for two-way communication and all the guests welcomed questions.
VMAC update
Dr. Wilson began her presentation by demonstrating where VMAC lies within the broader health authority structure. VMAC is one of three VCH medical advisory committees to report to HAMAC (the other two are Richmond and Coastal). In turn, HAMAC reports to the VCH Board of Directors. Medical staff associations such as VMDAS have a close affiliation with their medical advisory committee. MSAs are guided by rules and bylaws and represent the medical staff in their association.
VMAC’s role is to provide advice to VCH’s CEO and HAMAC on the quality of medical care in Vancouver Acute and Vancouver Community. This includes privileging, health-care resources, medical education, research, resources, and policy.
VMAC’s membership includes the chair (Dr. Wilson) and vice chair (Dr. Phil Dawe), senior medical directors, department heads, operations staff, community leadership, and VMDAS’s president. The committee meets monthly to share information and discuss policy changes. (VMAC and HAMAC meeting summaries are posted to VMDAS’s website and promoted via the weekly Checkup e-newsletter.)
Dr. Wilson noted that medical staff are often uncertain where to take their concerns. She suggested that members reach out to her or Dr. Dawe; if VMAC is not the right place for the issue, they can redirect it.
Current issues being addressed at VMAC include patient portals, medical education and how we treat learners in our health authority, and how we navigate non-beneficial care discussions.
Q: What is VMAC’s biggest challenge?
A: Making sure physician leadership has room at the table to voice concerns and the desire to create a more interactive space with time for brainstorming.
HAMAC update
Dr. Beaveridge introduced herself as HAMAC’s chair and referred to her vice-chair Dr. Anna McGuire, and HAMAC Coordinator Emily Holtorf-Ma. She went on to define HAMAC as a legally mandated governance body established by the BC Hospital Act and VCH Medical Staff Bylaws. Its functions are to advise the VCH board and CEO, provide governance of medical staff, and work in partnership with Medical Affairs. It provides recommendations and advice to the board and CEO in six key areas:
- Provision of medical care within VCH facilities and programs
- Monitoring of the quality and effectiveness of medical care provided within VCH facilities and programs
- Adequacy of medical staff resources
- Continuing education of the members of the medical staff
- Planning goals for meeting the medical care needs of the population served by VCH
- Recommendations to the board regarding all medical staff appointments
HAMAC is your voice. HAMAC’s 45 members include VCH senior leadership along with senior medical directors, regional department heads, medical advisory committee chairs, and VCH MSA presidents.
HAMAC’s core purpose is to ensure the delivery of safe, high quality patient care for our patient population by advising the board while keeping the frontline clinical perspective in mind.
Q: Medical staff rules are undergoing an update; when do you anticipate those will be available?
A: The rules have been difficult to update and ensure they meet the needs of the medical staff and the care that needs to be delivered. We’re moving it into a more iterative process so that it can be adaptable and moveable. The first subcommittee has been launched. We’re hoping to have the next iteration out in the coming months and are looking at ways to keep it useable and relevant.
Q: What goes to HAMAC rather than VMAC?
A: If it has regional impact, it should go to HAMAC. If it is a local priority or concern, it should go to VMAC.
Q: Master list of members?
A: Members are listed here.
Q: I am curious why many med staff continue to feel they don’t have a ‘voice’ at the table… is part of this a matter of communication/understanding of what HAMAC does? If you had a magic wand, what is one thing you might change in the way HAMAC functions?
A: I think overall I would like to dig a bit deeper to understand what having a voice means to medical staff. So, my magic wand solution would be to start with improved two-way engagement with medical staff to further understand.
Dr. Cheung reminded members that if they have questions/issues/concerns around the topics discussed at HAMAC or VMAC or would like to suggest new topics, please fill out this form.
Cerner Patient Portal and AI Scribes
Dr. Grafstein began his presentation with a 1936 quote from the New York Times: “A rocket will never be able to leave the Earth’s atmosphere.” It was an appropriate introduction to his discussion on the new CST patient portal named AccessMyHealth, noting that the portal will be a big change to the way we practice. He acknowledged that many have raised concerns but expects these issues will be resolved. Most other jurisdictions with electronic records have a patient portal; they share clinical information, and it makes patients happy and there is not a lot of impact to providers.
AccessMyHealth, which is scheduled to launch its first phase early in 2026, will be connected to CST Cerner. It will be accessible to patients from VCH, PHC, and PHSA. At that time, it will include the following key features:
- Login via the Health Gateway Platform (authenticated by a BC Services Card)
- Scheduled appointments
- Cardiology, lab, and medical imaging results
- Clinical documentation
- Allergies and procedure history
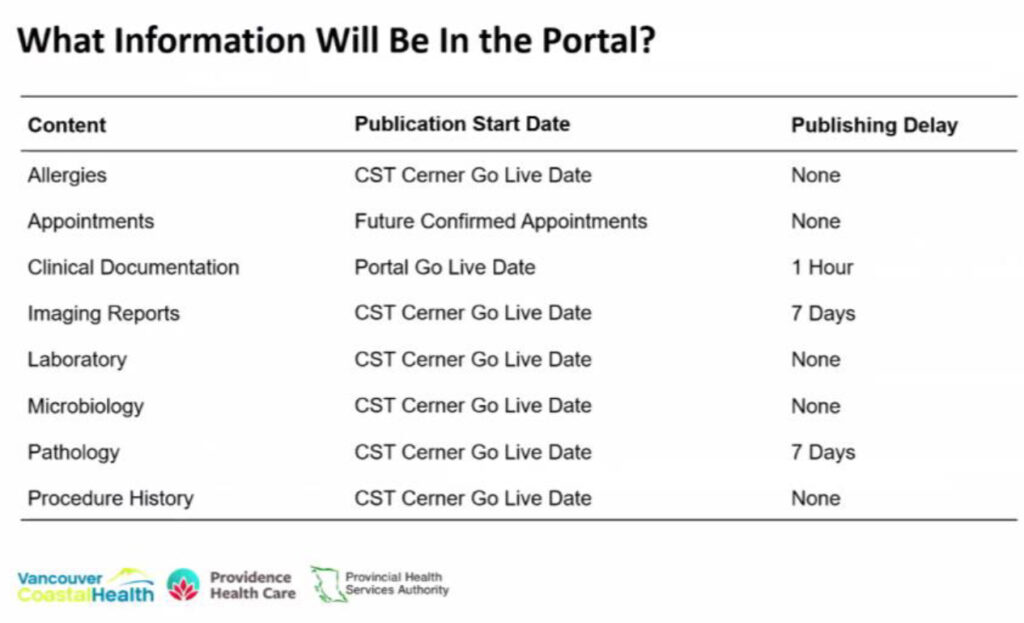 Dr. Grafstein emphasized the need to keep clinical documents factual and non-judgemental. The seven-day delay on posting imaging and pathology reports allows the primary care physician to talk with the patient about the results directly. He also addressed the contentious issue of patient proxies and how those apply to, for example, adolescents who request birth control prescriptions, or chlamydia testing, or a gender clinic. For this reason, patient proxies will be available to those under 12 and those over 18.
Dr. Grafstein emphasized the need to keep clinical documents factual and non-judgemental. The seven-day delay on posting imaging and pathology reports allows the primary care physician to talk with the patient about the results directly. He also addressed the contentious issue of patient proxies and how those apply to, for example, adolescents who request birth control prescriptions, or chlamydia testing, or a gender clinic. For this reason, patient proxies will be available to those under 12 and those over 18.
He summarized how CST Cerner documents will be distributed and noted the following:
- Documents will only publish to the portal from the go-live date forward.
- There will be a one-hour distribution delay on documents publishing to the portal.
- For individual situations where sending information to the portal could cause harm to the patient and/or a third party, a new note type (Provider Note – Do Not Distribute to Portal) will be available.
- The following note types (with some exceptions by medical speciality) will distribute to the portal:
- Consult notes
- Operative reports (TBC)
- Procedure notes
- Discharge summaries
- Clinic notes
- Patient handouts
Groups exempted are addiction medicine, adolescent medicine, child protection services, forensic psychiatry, perinatal addiction, psychiatry, and sexual assault services.
Medical staff education and notifications will be available via medical staff bulletins, a medical staff forum, CST Cerner Help, FAQs, e-Learning module (Best Practices in Documentation), and a medical staff PowerChart notification.
Dr. Grafstein also brought members up to date on the CST generative AI trial that involved four health authorities. He noted that these are expensive tools; the cost of MModal, which we currently use, is about $650,000/year for an enterprise licence. To use these tools at an enterprise level would be about $3-4 million a year, so it’s important to get a sense of their value. Close to 1,400 physicians signed up for cycle 1 of the trial, with nearly 1,000 signing up for cycle 2. The top three specialities in cycle 2 were psychiatry, family practice, and emergency.
There have been questions regarding why individual providers must pay for this rather than the organization. The cost and the value that we may get out of this is a real issue. This technology is potentially a game changer; to try to give people some advantage or some experience with it, VCH offered some trials and then offered the tool at a reduced rate. These tools, said Dr. Grafstein, work best if they are part of Cerner.
Q: Will reports that are generated outside of Cerner be pushed to Cerner (i.e., pathology reports written in CoPath) be available on the portal?
A: Yes.
Q: VCH has planetary health as one of its foundational pillars and we know AI is bad for the planet in terms of emissions. Has any consideration been given to mitigating that side of things as one of the unintended harms that could come from our use of this?
A: The good news is that AI technology is very expensive so there is a natural tendency to be very thoughtful about this. This is something that we need to continue to look into.
Q: Is there an approximate timeline on when there may be an AI agent integrated with CERNER?
A: No. We are piloting Cerner’s CAA Clinical AI Agent. That probably won’t start until January.
Q: Things are changing so quickly. I find stuff that I looked at a year ago is obsolete and even with these systems that we do take on that do integrate with Cerner, I feel that within a year there’ll be something much faster, better and more effective. So, what’s the plan to continuously evaluate that?
A: Having something that is amazing and works well is only half of the solution. The other half needs to be, is this a stable company? Do they provide good customer service? Are they innovating? Are they new, or old and stale? Are they going to be around in 10 years or bought out by someone else? That’s what happened to MModal. They’ve been bought and sold twice since we purchased their software. You have to have a partner that is on top of things.
Q: Will there be any guidance available for specific provider/note types that utilize medical jargon (i.e., pathology reports again) to ensure that our reports are still complete/following our guidelines, but don’t generate additional work for our clinical colleagues walking their patients through every line?
A: The fact that there’s technical jargon, that’s OK. I don’t think the expectation is for providers to change those notes to make them understandable for patients. They can talk to their family doctor or pass things through ChatGPT.
Q: It is foreseeable that this change will result in an increased amount of communication from patients to medical leadership? Is the health authority going to provide any support staff to help filter out and direct comments and complaints to help ensure that department heads (who already deal with a lot) aren’t faced with a significantly increased workload?
A: This is the concern… that patients are going to respond to these notes and complain. There is a process now through Medical Records. We’re going to use this same machinery to deal with these complaints and see how it goes.
Q: Can you choose to turn on the portal if you want to use it as a mechanism of communication?
A: Not right now.
Q: Fifteen to 40 per cent of radiology reports have incidental findings. Is there an anticipated increase in medical questions and testing because of this?
A: If there are incidental findings that need follow up, patients having their information may help close the loop. I think empowering patients to say something when they notice something can be helpful.
Q: A big part of my job as a geriatrician is intimate description of caregiver stress about patients. How can I protect this confidential part of the conversation while this belongs to the patient’s record?
A: This is a good question. It is a common thread “how do I know that the information I might be sharing is too sensitive or might cause too much harm.” There is no obvious right answer here. There are, however, a couple of things to keep in mind. The first is that there have been relatively few complaints related to this sort of issue around release of sensitive information. When I spoke to CMPA, this type of content has not come up as a significant college or legal issue.
The second point is that we live in a changing world. It is increasingly the patient’s expectation that they will be able to see their information. This happens all over the world. We are among the last jurisdictions to implement a portal. As well, many patients are requesting their information from Medical Records. It is important to note that, regardless of whether or not you create a note that you think is sensitive, the patient is allowed to see that information. There are, however, some exceptions, for example, cases that involve the Adult Guardianship Act. This is an example where there is significant risk of substantial harm. I do note that putting some of that very focussed content in a do-not-distribute note might be helpful for Medical Records to understand what you feel is sensitive.
In summary, there are not many examples where the sharing of this “sensitive “information has been an issue for providers or patients. We will pay close attention to how the sharing of documents in the portal unfolds. If we need to course correct after go live, we will.
Upcoming events
VMDAS’s annual awards will be presented on November 17. The MSA’s and VPSA’s joint annual general meetings will be held December 8.
Photo caption (from left): VMDAS Past President Dr. Alison Harris, guest speaker Dr. Eric Grafstein, guest speaker Dr. Jennifer Wilson, and VMDAS President Dr. Ka Wai Cheung.